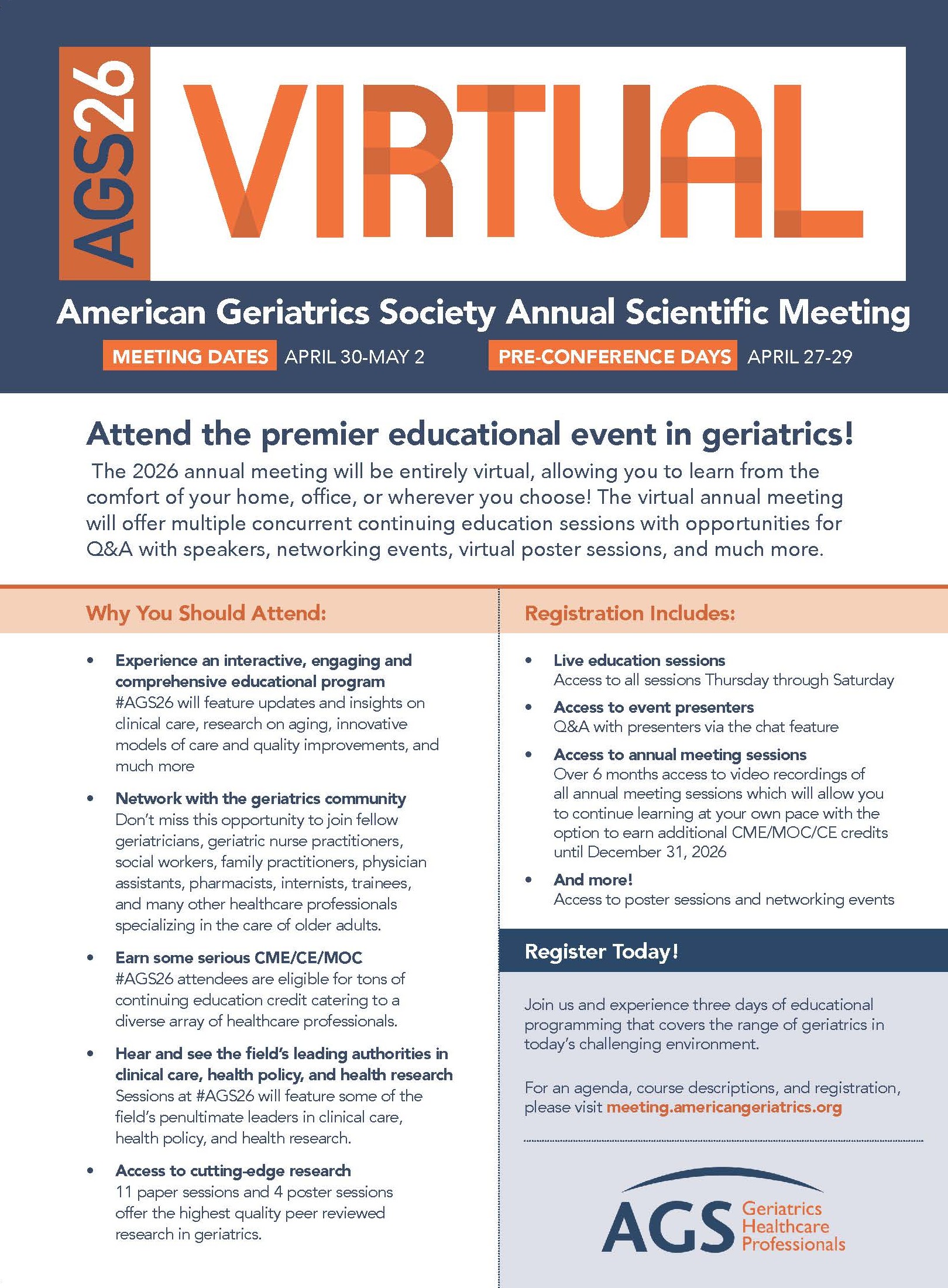
The American Geriatrics Society is excited to invite you to the 2026 AGS Annual Scientific Meeting, taking place virtually from April 30th–May 2nd, 2026 (with pre-conference sessions starting on April 27th). #AGS26 will bring together geriatrics professionals from around the world for a program full of opportunities to learn, collaborate, and connect—no travel required.
The AGS Annual Scientific Meeting remains the premier event in geriatrics education, featuring the latest advances in clinical care, aging research, and innovative models of care delivery. This year’s virtual meeting format provides attendees with the flexibility and accessibility that allows them to attend more sessions. The #AGS26 platform will remain open until the end of 2026, which means that registrants will have more time to view sessions and get CME. Like past Virtual Annual Meetings, participants attending the simu-live sessions April 30th–May 2nd can engage with speakers via the live chat for questions and answers.
Going virtual also brings practical advantages: reduced travel costs, easier access for those with demanding clinical schedules, and the ability to extend participation to a wider audience of geriatrics professionals. Plus, the virtual meeting significantly reduces our environmental impact, aligning with AGS’s commitment to sustainability and innovation.
And while we won’t be gathering in person, there will be no shortage of opportunities for real-time interaction. Attendees can engage directly with poster presenters during multiple live sessions, join likeminded colleagues for passionate discussions in Special Interest Group meetings, and participate in virtual mentoring opportunities. “Virtual meetings like #AGS26 expand the reach of our community,” said Program Chair Nicole J. Brandt, PharmD, MBA, BCGP, FASCP. “They make it easier than ever to share knowledge, exchange ideas, and engage with colleagues from around the world. Whether you’re joining from your office, clinic, or home, you’ll experience the same spirit of collaboration and excellence that defines every AGS meeting."
Join us online for #AGS26 to advance your practice, connect with peers, and explore the future of geriatrics from wherever you are.
Sessions Preview
Physicians, nurse practitioners, nurses, pharmacists, physician assistants, social workers, long-term and managed care providers, healthcare administrators, and other professionals committed to improving care for older adults are all welcome to attend. Sessions covering a range of topics will run during the meeting, representing the breadth and depth of subjects relevant to geriatrics. The following is a small sample of topics that will be presented.
Artificial Intelligence in Geriatrics: Innovations in Research and Clinical Practice
As the aging population grows, AI holds promise for advancing both the science of aging and the delivery of age-friendly, data-driven care, ultimately contributing to improved health span and quality of life for older adults. This symposium will target clinicians, researchers, and other interprofessional members, including a broad audience of any health professional from any discipline who has learned or is interested in learning how to work collaboratively with either computer scientists or engineers, and potential examples as to how to integrate such technologies to improve patient care.
Navigating SGLT2 inhibitors and GLP-1 Agonists use in the Older Adult: A Guide to Benefits, Risks, and Shared Decision-Making
Current guidelines recommend use of SGLT2 inhibitors and GLP-1 agonists for management of type 2 diabetes and heart failure. Recent data shows that these agents can delay progression of chronic kidney disease. However, these guidelines do not specifically address when to initiate these medications in older adults, how to manage side effects, or when to de-intensify. The purpose of this symposium is to address the professional practice gap in the practice of prescribing and management of SGLT2 inhibitors and GLP-1 agonists in older adults with chronic kidney disease and geriatric syndromes.
Acute Illness, Resilient Responses: Advancing Physical Resilience in Geriatric Acute Care
This symposium will explore innovative approaches to understanding and predicting physical resilience in older adults within acute care settings. Anchored by a newly proposed conceptual framework of physical resilience in geriatric medicine, the session will integrate perspectives from clinical research, data science, and emerging technologies to highlight how resilience can be measured, monitored, and supported during episodes of acute illness.
Dysphagia in Hospitalized Older Adults: Clinical Challenges, Cultural Contexts, and the Geriatrician’s Role in Shaping Solutions
Dysphagia is a common and often complex symptom in hospitalized older adults, particularly when compounded by delirium and dementia. Managing oropharyngeal dysphagia in this context presents unique challenges, as both dysphagia and aspiration risk can severely impact nutritional intake and contribute to malnutrition leading to further complications. This presentation highlights challenges, raises awareness among attendees about similar issues in their own institutions, and proposes practical, evidence-based solutions.
Connected from Anywhere
“By embracing the virtual platform, we expand access for many geriatrics professionals and trainees to join from anywhere, balance their clinical and personal commitments, and still engage meaningfully with colleagues, relevant clinical updates, and new research. It’s rewarding to know that whether we’re meeting on screen or in person, our shared dedication to improving care for older adults keeps us deeply connected,” shared Program Chair Nicole J. Brandt, PharmD, MBA, BCGP, FASCP.
Follow #AGS26 for Updates!
Use the hashtags #AGS26 and #AGSProud to spread the word about your meeting plans and to connect with other attendees online. Look for updates from @AmerGeriatrics, @AGSJournal, @HealthinAging, and AGS CEO @NLundebjerg to remain in-the-know about all things #AGS26. Plus, remember to follow meeting updates on MyAGSOnline and the AGS Week-in-Review, as well as the AGS and Annual Meeting Websites.

 I'Il confess that I’ve been having a bit of writer’s block since I started to write this column on the train from New York City to Washington, DC to attend the ClinSTAR and Council of Medical Specialty Societies meetings. ClinSTAR is up first – it’s a great opportunity for me to celebrate all of the young people who are electing to pursue careers in aging research. The second meeting includes a gathering of the CEOs of medical specialty societies - over the years, I’ve learned so much from this gathering and can’t wait to participate again.
I'Il confess that I’ve been having a bit of writer’s block since I started to write this column on the train from New York City to Washington, DC to attend the ClinSTAR and Council of Medical Specialty Societies meetings. ClinSTAR is up first – it’s a great opportunity for me to celebrate all of the young people who are electing to pursue careers in aging research. The second meeting includes a gathering of the CEOs of medical specialty societies - over the years, I’ve learned so much from this gathering and can’t wait to participate again.